Medical concerns must determine vaccine distribution
As COVID-19 vaccines have become available, the question has been asked ‘Who gets them first?’
We want to be lead by ‘the science’ and that tells us that “Vaccinating older adults for COVID-19 first will save substantially more U.S. lives than prioritizing other age groups.” This makes sense given what we know about who COVID-19 hits hardest. Back in August, I noted that:
It is care home residents, people aged 70 and over, Native Americans and, to a lesser extent, Asians who are at a higher risk of an infection becoming acute and resulting in hospitalization, ICU care, or death.
This is still the case. Given the apparently high number of asymptomatic cases, it is hard to know for sure whether certain demographic groups are more or less likely to be infected with COVID-19. But we can look at how likely a diagnosed case is to become acute – to require a hospital stay, ICU care, or result in death.
Figure 1 summarizes this Department of Health information up to March 11. It shows that, in terms of the characteristics which predict whether a diagnosed case of COVID-19 will result in death, nothing comes close the age of the person infected. For those aged 85 and over, nearly a quarter of diagnoses result in death. For the highest non-age related category, ‘Amer. Indian/AK Native, NH,’ 1.9% of diagnosed cases result in death.
Figure 1: Percentage of diagnosed COVID-19 cases resulting in death in Minnesota
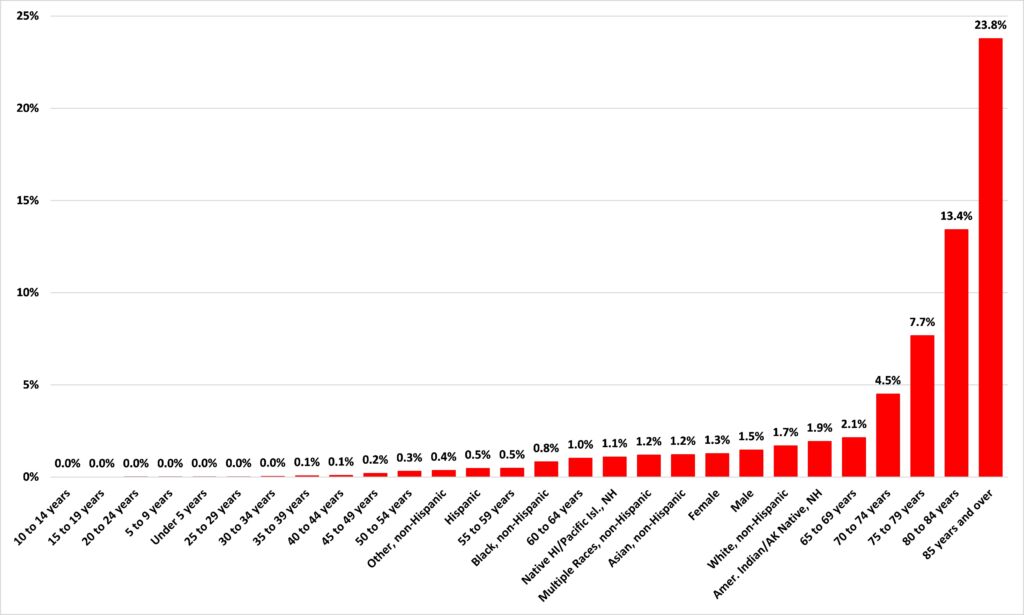
Source: Minnesota Department of Health
So, if we want to save the most lives, we should prioritize people for vaccine distribution by age. Broadly speaking, that is what the state has been doing.
But this has not satisfied some. In February, the Star Tribune reported: ‘Minnesota falling behind in equitable allocation of COVID-19 vaccine‘:
Minnesota has strayed from its commitment to distribute the COVID-19 vaccine to communities that are among the highest risk for severe disease and death, according to three members of the state’s vaccine allocation advisory panel.
They are joined by 350 clinicians, researchers and organizations that sent a letter to state officials this week raising concerns that the state has not prioritized vaccines for Black, Indigenous, Hispanic and Asian Minnesotans.
As the Department of Health data shows, the communities that are “the highest risk for severe disease and death” are Minnesotans aged over 65, especially those aged over 70. The article went on:
…some on the vaccine panel were surprised when state leaders took the rollout in an unexpected direction, expanding eligibility to seniors 65 and older, as well as school and child-care workers.
Again, as the data show, if we want to save the most lives prioritizing over 65s is exactly what the state ought to be doing.
A couple of weeks ago, MPR News reported:
More than two months into Minnesota’s COVID-19 vaccination rollout, the state Health Department has released long-awaited data on the race and ethnicity of the people who so far have been vaccinated, most of whom have been 65 or older.
For people of color in the state age 65 and older, the percentage of people receiving vaccinations is trailing slightly their share of the state’s population.
Is it? Not according to data from the Department of Health. As Figure 2 shows, as of March 17, White Minnesotans, who make up 94.2% of the state’s population aged over 65, make up 94.9% of the over 65s vaccinated in the state. That isn’t much of a discrepancy.
Figure 2:
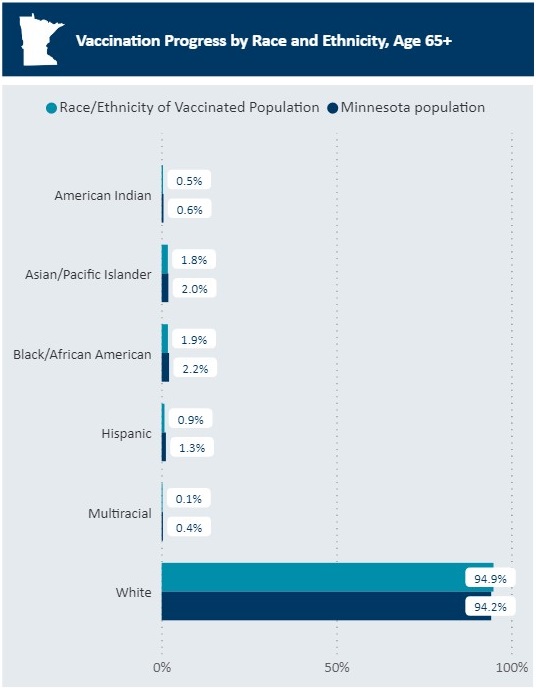
Source: Minnesota Department of Health
COVID-19 is not an equitable virus. As I’ve written before, it is “like a laser guided missile designed to kill the elderly, especially those in care homes.” If we are serious about saving the most lives, age and care home residency are the criteria we ought to be using. Those who argue that we should use some other criteria are saying, in effect, that saving the most lives is not their main priority. To be blunt: vaccinating those in lower risk groups is nothing less than condemning some in higher risk groups to death in the name of ‘equity.’
John Phelan is an economist at the Center of the American Experiment.